Oncology
Chimeric Antigen Receptor (CAR) T cell therapy has shown great promise for cancer treatment.
Oncology is a critical branch of medical research that specialises in the treatment and diagnosis of cancer. This involves a range of sub-categories including medical, radiation and surgical oncology, each of which are studied and utilised based on a range of scenarios. Millions of people are living with the struggles of cancer and have been for years, whether it is family, friends or themselves, but contemporary advancements and research mean the weight and pain can be slightly lifted from those affected [1].
Diagnostics plays a key part in cancer research and oncology, being able to discover and diagnose cancer in its early stages can make the difference between life and death. This is why, the most commonly used methods of diagnosis, cancer biopsies and tissue examinations, must be carried out utilising the most time-efficient and accurate methods. There are several other methods of diagnosis including endoscopy for the gastrointestinal tract and imaging tests including computerised tomography (CT), bone scan, magnetic resonance imaging (MRI), positron emission tomography (PET), ultrasound and x-rays [2].
CAR T Cell Therapy
With regards to contemporary methods of cancer-fighting, there have been several breakthroughs that provide hope for those suffering from cancer or with a genetic predisposition to the tumour. The first of which is CAR-T targeted immunotherapies which harness and utilise the power of the body’s immune system to attack cancer cells. T cells play a vital part in the body’s immune system, but these T cells are unable to differentiate between cancer cells and regular cells and therefore the malignant tumour continues to grow, invade organs and absorb sugars and amino acids from neighbouring cells.
To alter these cells, a process called apheresis takes place where T cells are removed from the blood, they are then expanded and genetically modified in a laboratory where they become CAR-T cells (chimeric antigen receptor T cells) resulting in enhanced antigen specificity. This is done by activating the T cells via aAPCs (artificial antigen-presenting cells) and transducing these with a CAR-encoding viral vector resulting in the modification of genetics to express the desired antigen detection, after which they are expanded to large numbers via the use of a bioreactor. Once they have multiplied, they are administered back to the patient where the cancer is present; only at this point, the altered T cells are able to differentiate between healthy cells and cancer cells, therefore meaning that CAR-T cells are able to recognise and attack these harmful tumours. This method of therapy is currently only available for some children with leukaemia and some adults with lymphoma, depending on a wide range of varying circumstances which are detailed on Cancer Research UK’s website [3,4].
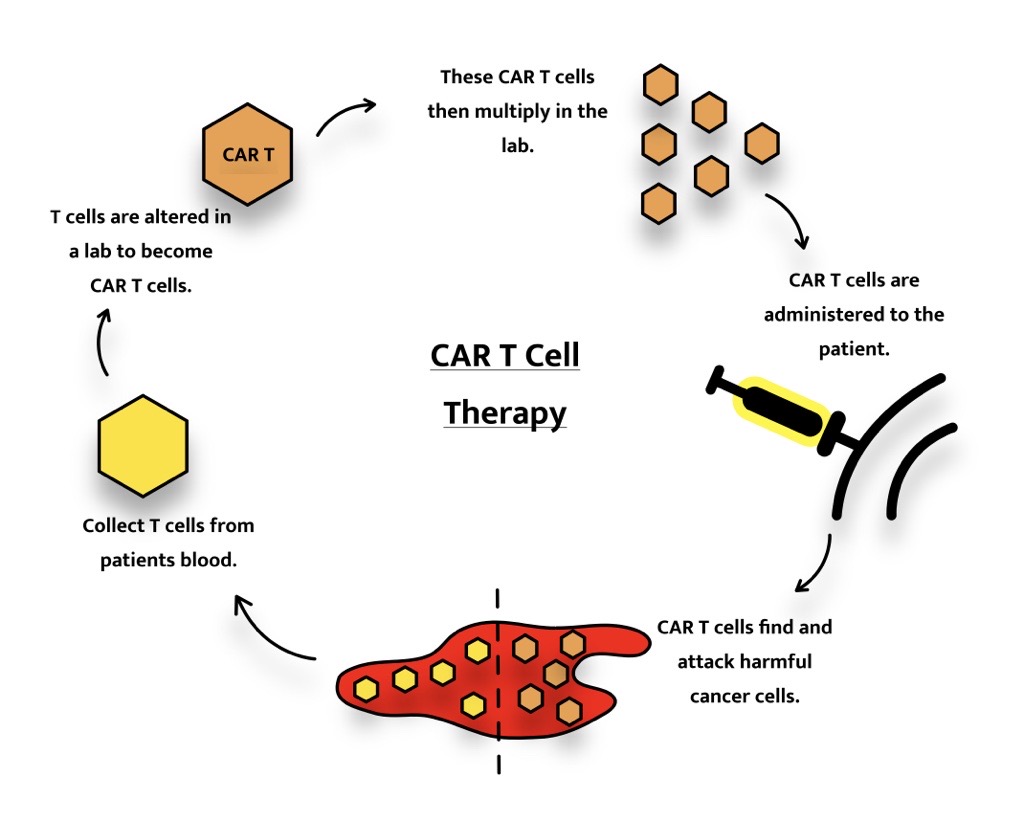
With regards to contemporary methods of cancer-fighting, there have been several breakthroughs that provide hope for those suffering from cancer or with a genetic predisposition to the tumour. The first of which is CAR-T targeted immunotherapies which harness and utilise the power of the body’s immune system to attack cancer cells. T cells play a vital part in the body’s immune system, but these T cells are unable to differentiate between cancer cells and regular cells and therefore the malignant tumour continues to grow, invade organs and absorb sugars and amino acids from neighbouring cells. To alter these cells, a process called apheresis takes place where T cells are removed from the blood, they are then expanded and genetically modified in a laboratory where they become CAR-T cells (chimeric antigen receptor T cells) resulting in enhanced antigen specificity. This is done by activating the T cells via aAPCs (artificial antigen-presenting cells) and transducing these with a CAR-encoding viral vector resulting in the modification of genetics to express the desired antigen detection, after which they are expanded to large numbers via the use of a bioreactor. Once they have multiplied, they are administered back to the patient where the cancer is present; only at this point, the altered T cells are able to differentiate between healthy cells and cancer cells, therefore meaning that CAR-T cells are able to recognise and attack these harmful tumours. This method of therapy is currently only available for some children with leukaemia and some adults with lymphoma, depending on a wide range of varying circumstances which are detailed on Cancer Research UK’s website [3,4].
Targeted Therapies
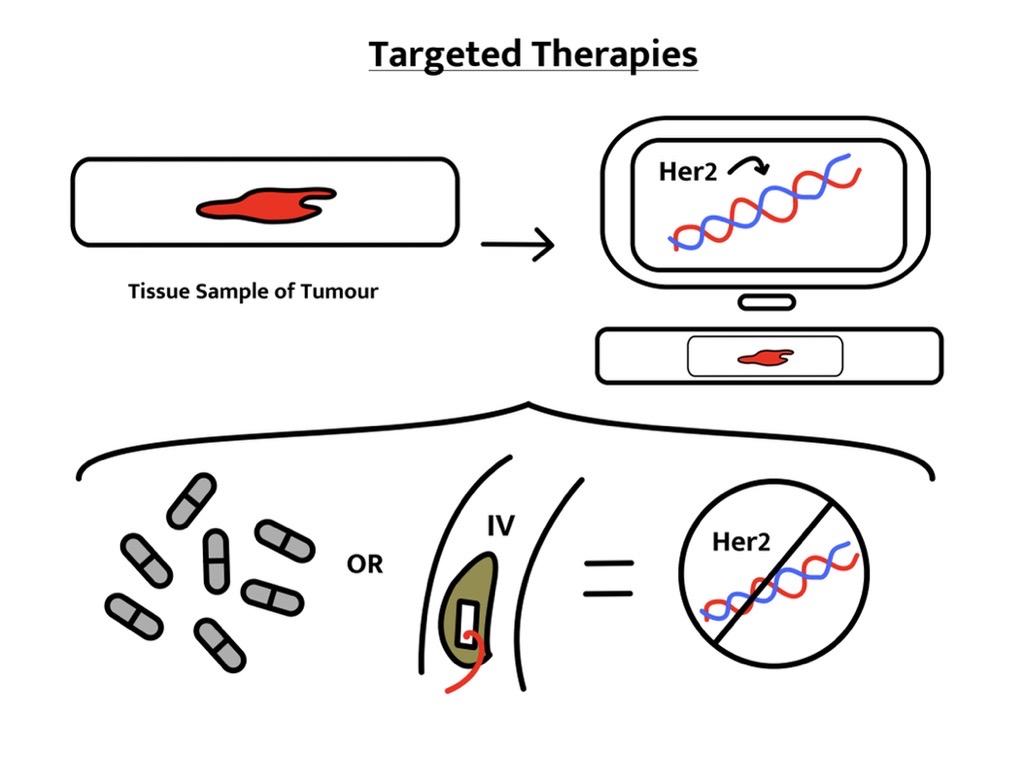
Another less intrusive method of cancer treatment is that of targeted therapies, these begin by assessing the genetic profile of present cancer to be able to target the specific genes that caused the tumour’s development. From this, genes that promote the spread of the tumour are established and medication can be administered in the form of a course of pills or via IV (Intravenous) and can be carried out at any stage during the growth of the tumour. A significant advantage of this is that healthy cells are not harmed in the process which can prevent negative, life-altering implications. This means that research and studies regarding how this methodology can be utilised are vital in progressing cancer treatment [6].
2BScientific Limited has a range of products, including a selection of cancer research-based products. 2BScientific is passionate about ensuring that customers get the precise, required product and have a friendly and knowledgeable team ready to answer any technical queries.